A powerful movement to overhaul how the National Health Service treats its workforce is gaining unprecedented momentum, born from the ashes of a devastating personal tragedy. At the heart of this campaign is Amin Abdullah, a 41-year-old award-winning nurse whose life and career ended in a manner that continues to haunt the medical community. Today, prominent whistleblowers and healthcare advocates are calling on NHS England to implement "Amin’s Rule"—a mandatory independent second opinion for all staff dismissals—to ensure that no other professional is driven to the same desperate end.
The Journey of an Award-Winning Caregiver
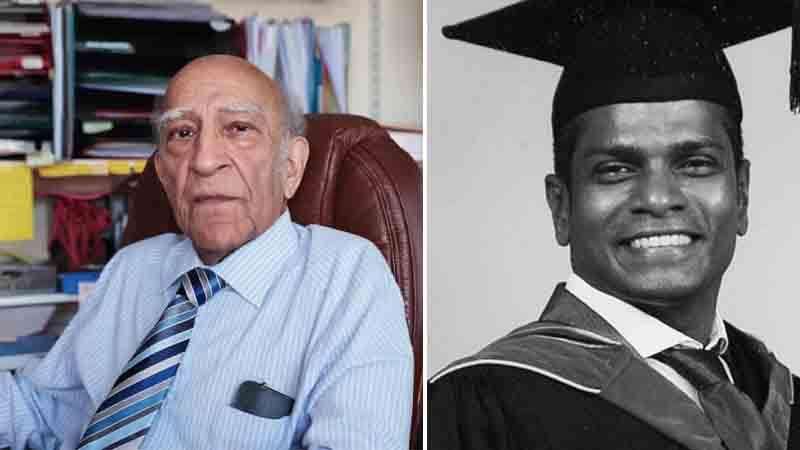
Amin Abdullah’s path to the frontlines of British healthcare was defined by extraordinary resilience. Born in Malaysia and raised in an orphanage in Kuala Lumpur, Abdullah arrived in the United Kingdom in 2003 with a singular dream: to dedicate his life to nursing. His commitment was undeniable; he graduated with honors from Buckinghamshire New University and won the prestigious Hannah Evans Award for Excellence. Colleagues at Charing Cross Hospital described him as a deeply compassionate deputy ward manager who "lived for the job." He shared a quiet, stable life in Notting Hill with his partner of 12 years, Terry Skitmore, and had become a proud British citizen in 2009.
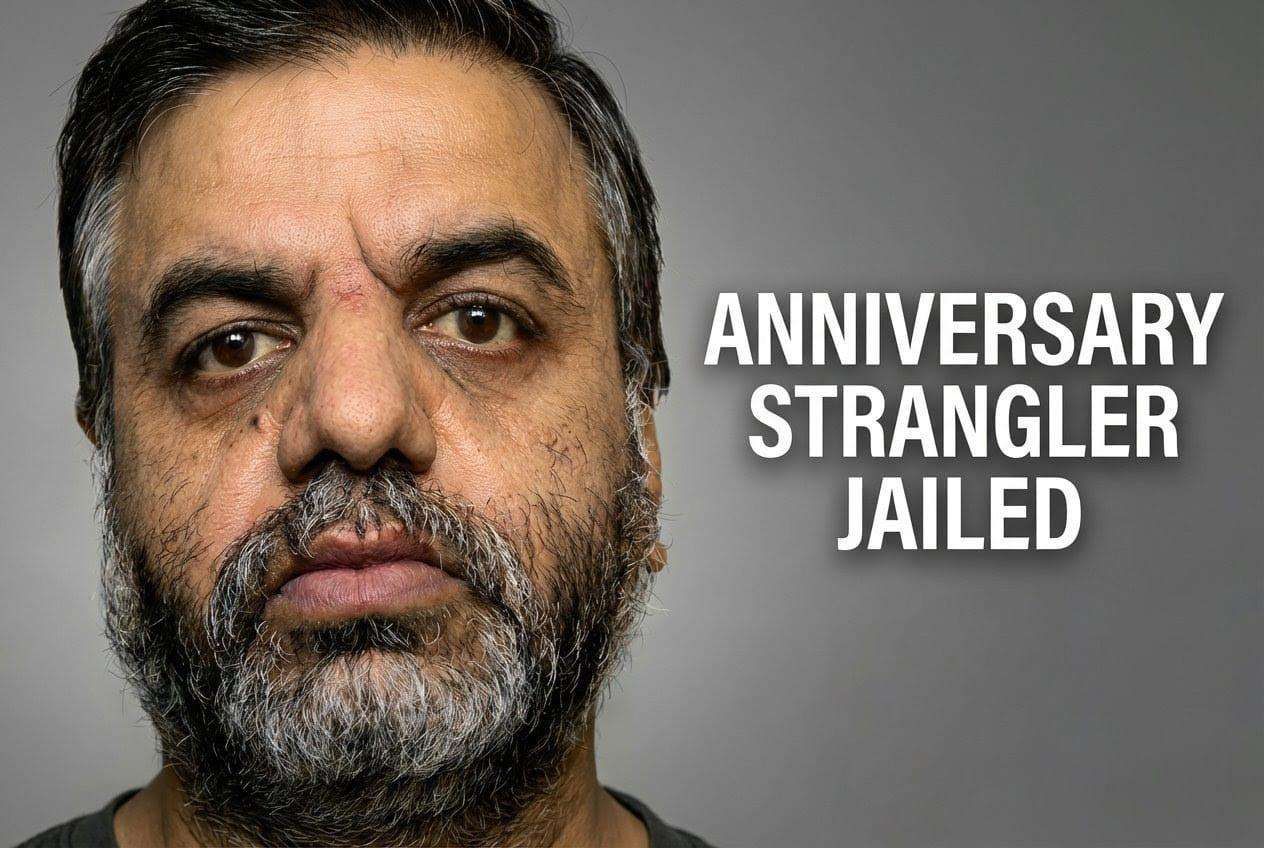
However, this life of service was derailed by what supporters call a "kangaroo court" disciplinary process. In 2015, Abdullah was suspended for signing a petition and writing a letter in support of a colleague during a patient dispute. Despite his unblemished record and the fact that 18 other colleagues signed the same petition without facing discipline, Abdullah was singled out. The psychological weight of the five-month investigation and his subsequent summary dismissal for "gross misconduct" shattered his mental health. In February 2016, just two days before his appeal was to be heard, he set himself on fire outside Kensington Palace.
Confronting Systemic Bias and Racial Disparity
The push for Amin’s Law, led by Dr. Narinder Kapur, is rooted in alarming evidence regarding the treatment of ethnic minority staff within the NHS. Dr. Kapur, a consultant neuropsychologist who was himself unfairly dismissed after raising safety concerns, argues that the current system lacks the objectivity required to protect minority professionals from systemic bias. Official data consistently shows that Black and Minority Ethnic (BME) staff are significantly more likely to face formal disciplinary action than their white counterparts. An independent inquiry into Abdullah’s case later confirmed he had been "treated unfairly," with investigators repeatedly questioning his honesty based on "little or no evidence."
By introducing an external, independent arbiter into the dismissal process, advocates believe the NHS can eliminate the weaponization of disciplinary procedures. The reform specifically targets the "Some Other Substantial Reason" (SOSR) legal loophole, a mechanism used to terminate over 10,000 NHS contracts between 2010 and 2018, often citing a "breakdown in relationships." For whistleblowers and BME staff, this clause has frequently served as a tool for institutional retaliation rather than a measure of professional capability.
A New Framework for Healthcare Accountability
The proposed reforms extend beyond a single rule to a fundamental restructuring of healthcare regulation. Campaigners are calling for the Care Quality Commission (CQC) to be split into two distinct entities: one focused on patient safety and the other dedicated entirely to staff welfare and the protection of whistleblowers. This dual-oversight model is designed to ensure that the rights of those who provide care are as protected as the patients who receive it.
As NHS England enters high-level discussions regarding these changes, the legacy of Amin Abdullah serves as a grim reminder of the human cost of administrative failure. For his partner, Terry Skitmore, and the thousands of healthcare workers currently fearing for their careers, "Amin’s Law" represents a necessary evolution toward a more just, transparent, and humane National Health Service. The implementation of an independent second opinion would finally offer a safeguard for the dedicated professionals who, like Amin, give everything to their patients but find themselves abandoned by the system they serve.






.svg)

_1.jpg)
_1.jpg)